Diabetes affects 450 million people worldwide and about 7% of those (more than 32 million) are Americans. Diabetes, a disease itself, also raises the likeliness of contracting many different diseases that affect nearly every organ system in the human body. These diseases include kidney failure, coronary heart disease, stroke, and even blindness, among many others. Diabetes has also been found to increase the risk of severe symptoms of COVID-19, the disease caused by the ongoing coronavirus pandemic.
The University of California has pulled off one amazing feat of software engineering by using a smartphone camera to diagnose type 2 diabetes with a high degree of accuracy. The researchers demonstrated a method that needs no hardware other than a functional smartphone and smartphone camera. At the moment, the system they have engineered is just over 80 percent accurate in detecting Type II diabetes. If you think about that for just a second, that is simply amazing. The fact that smartphones, software design, and just humans, in general, have progressed to the point in which a common device can detect a deadly disease is simply astonishing.
This is clearly a good thing. This software is still in development and is already 80% accurate. That’s only going to get higher. Lead author of the study, Robert Avram said, ‘Diabetes can be asymptomatic for a long period of time, making it much harder to diagnose. To date, noninvasive and widely-scalable tools to detect diabetes have been lacking, motivating us to develop this algorithm.’
The University of California system is based on something called PPG (photoplethysmography). PPG is a technique where photons from a light source are directed into tissues so that changes in blood volume can be detected. The most common scenario in which the public comes into contact with PPG technology is their doctor uses a small finger clamp to measure blood oxygen levels and heart rate.
As the smartphone revolution happened and high-brightness LED flashes became more and more commonplace, researchers quickly saw that the newly pervasive devices could be used to capture PPG data. In this study, the University of California hypothesized that by using smartphone-acquired PPG measurements, they should be able to detect diabetes by way of the damage that it does to someone’s vascular system. Well, they were right.
Geoffrey Tison, co-senior author of the study said, ‘The ability to detect a condition like diabetes that has so many severe health consequences using a painless, smartphone-based test raises so many possibilities. The vision would be for a tool like this to assist in identifying people at higher risk of having diabetes, ultimately helping to decrease the prevalence of undiagnosed diabetes.’
The first part of the process involved using AI to create a deep-learning algorithm that was able to go through the millions of PPG recordings required to be able to find out if the vascular biomarker could in fact identify whether or not people had diabetes. The deep neural vascular network was trained by inputting 2.6 million PPG recordings into it from 53,870 individuals that had been positively diagnosed with diabetes.
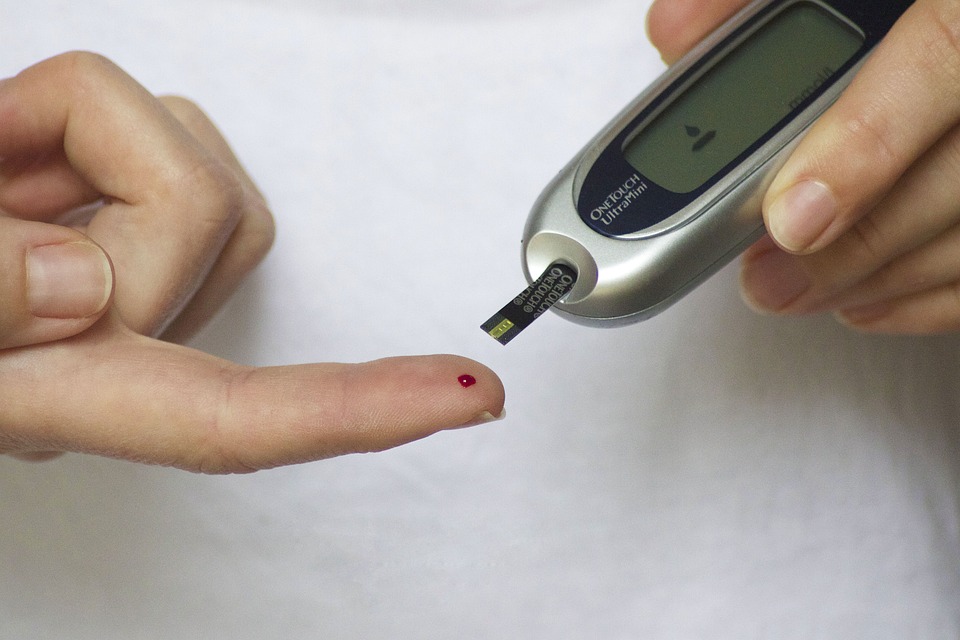
After the algorithm was in place, the University of California researchers then tested its ability to make a positive determination of diabetes using nothing but a common smartphone’s PPG data in three independent groups. The data was gathered by pressing the device’s flashlight and camera to the patient’s fingertips. The AI network was able to then accurately detect diabetes in about 80% of subjects. The algorithm was able to make even better predictions when combined with other basic patient data such as weight, age, and height.
Jeffrey Olgin, another author mentioned, ‘We demonstrated that the algorithm’s performance is comparable to other commonly used tests, such as mammography for breast cancer or cervical cytology for cervical cancer, and its painlessness makes it attractive for repeated testing. A widely accessible smartphone-based tool like this could be used to identify and encourage individuals at higher risk of having prevalent diabetes to seek medical care and obtain a low-cost confirmatory test.’
Of course, it’s going to take a while before this breakthrough translates into any kind of real-world diabetes-detecting app, but what it does mean, is that we are inching closer and closer to our smartphones functioning a lot like Star Trek Tricorders. The researcher’s best bet to get this thing off the ground, or out of the lab, rather, is to see just how this particular tool of theirs can be effectively integrated into the existing system of diabetes screening practices.

